Author: Nina Isoherranen, PhD on September 20, 2017 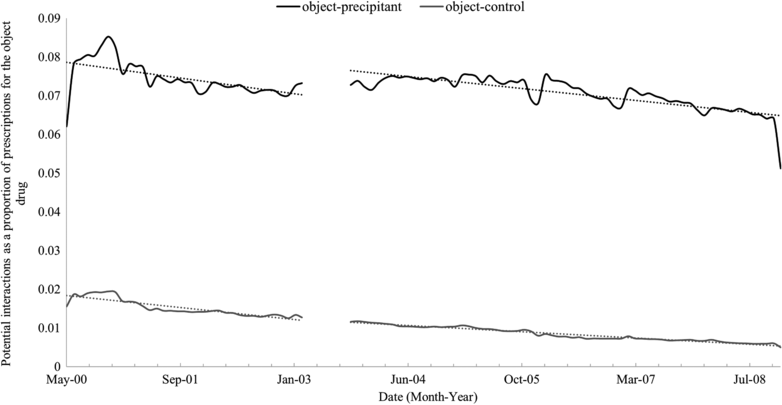
Several analyses have previously demonstrated the delay of translating new information of clinically significant drug-drug interactions (DDIs) to drug labels, and the lack of consistency of drug-drug interaction labeling between the interacting drugs. The brief report “Lost in Translation: No Effect of a High-Profile Publication on the Concomitant Use of Interactive Drugs,” published in Clinical and Translational Science in July 2017, further highlights this translation gap of bringing cutting edge new information of potentially serious DDIs consistently into clinical practice.
The report specifically focuses on the clinical translation of DDI studies that demonstrate serious clinical consequences. The DDIs evaluated included ACE inhibitors with potassium-sparing diuretics, digoxin with clarithromycin, and glyburide with cotrimoxazole (sulfamethoxazole/trimethoprim). Each of these combinations had been previously identified to result in DDIs, and a single high-profile publication demonstrated that they were strongly associated with adverse events and hospitalizations.1 The paper in CTS shows that the publication of the significant DDIs had minimal to no effect in the prescribing practices of these medications.
It is noteworthy that, even still in 2017, the product label of glyburide does not mention the specific drug interaction with sulfamethoxazole/trimethoprim but broadly refers to sulfonamides in the list of drugs that may increase the hypoglycemic effect of sulfonylureas. The lack of translation of even very high-profile DDI papers into clinical practice is worrisome for all scientists working in this field. Major advances have been made in the area of predicting and quantifying DDIs, and at present this is a mature science that could be readily applied. Yet, multiple publications have demonstrated that major barriers exist for translation, including prescriber’s poor knowledge and understanding of DDIs, and DDI alert fatigue with pharmacists and prescribers. The alert fatigue is a particularly concerning issue resulting in potentially fatal combinations of medications to be prescribed and dispensed. As recently as December 2016, an investigative report in the Chicago Tribune showed that 52% of DDIs labelled as dangerous drug combinations were missed by the pharmacists filling the prescription.
These CTS authors offer a solution to the situation suggesting that the overall quality and signal-to-noise ratio of DDI knowledge bases needs to be improved to translate the rich science of DDIs into clinical practice. At the same time, we need to invest more strongly on the education of physicians and pharmacists on DDIs starting from the science of drug-drug interactions
Reference:
1. Juurlink DN et al. Drug-drug interactions among elderly patients hospitalized for drug toxicity. JAMA. 289, 1652-1658 (2003).
Image by Acton, et al. Clin. Trans. Sci., doi: 10.1111/cts.12494, is licensed under CC BY-NC 4.0. ©2017 The authors.

The comment feature is locked by administrator.