Author: Cameron D. Thomas, PharmD; Jean G. Malave, PharmD; Larisa Cavallari, PharmD on August 16, 2024 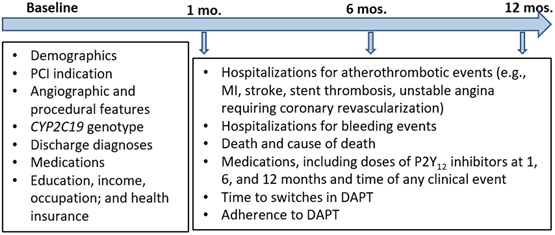
Antiplatelet therapy is crucial after percutaneous coronary intervention (PCI), a common procedure used to open blocked coronary arteries, to prevent a heart attack, stroke, or death. However, antiplatelet therapy is associated with increased risk for bleeding, leading to adverse effects for patients. In addition, the effectiveness of antiplatelet therapy varies significantly across patients. Over the last decade, there have been significant strides in tailoring antiplatelet therapy based on a patient’s genetic makeup in an effort to improve treatment effectiveness and reduce bleeding risk. In particular, genotyping for variants in the CYP2C19 enzyme is now done at an increasing number of medical centers to help with selection of antiplatelet therapy. Cavallari et al. describe a multi-center study, called Precision PCI, that aims to enhance our understanding of how genetic and patient-specific factors influence the effectiveness of antiplatelet therapy. This paper is an example of a new category at Clinical and Translational Science, Clinical Trials in Progress, which covers substantial novel original research protocols. The study addresses critical gaps in our understanding of outcomes and factors influencing outcomes with genotype-guided antiplatelet therapy, particularly in a diverse, real-world patient population.
Research teams at three U.S. medical centers have been collecting data and genetic samples from patients who were genotyped as part of their clinical care to guide antiplatelet therapy after PCI. One of the most significant contributions of this study is its focus on outcomes in Black patients, who were underrepresented in previous studies. The study will also examine the effectiveness of reducing the intensity of antiplatelet therapy in patients with certain genotypes in an effort to reduce bleeding risk. This is crucial because randomized controlled trials have shown mixed results with genotype-guided therapy, yet there are gaps regarding outcomes in high-risk, diverse, real-world populations.
As of early 2024, data have been collected for more than 5,500 patients with genetic samples available for nearly 2,500 patients. The comprehensive data collection, including from electronic health record reviews and patient interviews, promises to inform studies of real-world effectiveness of genotype-guided antiplatelet therapy, including in self-reported Black or African American patients. Beyond the immediate clinical implications of these findings, the Precision-PCI study aims to expand our understanding of genetic associations with clopidogrel response by investigating genetic variants beyond the well-known CYP2C19 alleles. Thus, this study promises to uncover new genetic variants associated with response to antiplatelet therapy. As we move towards more personalized approaches in cardiovascular medicine, the findings from this study are expected to inform targeted antiplatelet drug selection strategies, ultimately leading to improved clinical outcomes for patients undergoing PCI.

The comment feature is locked by administrator.