Author: Valentina Shakhnovich, MD on July 12, 2019 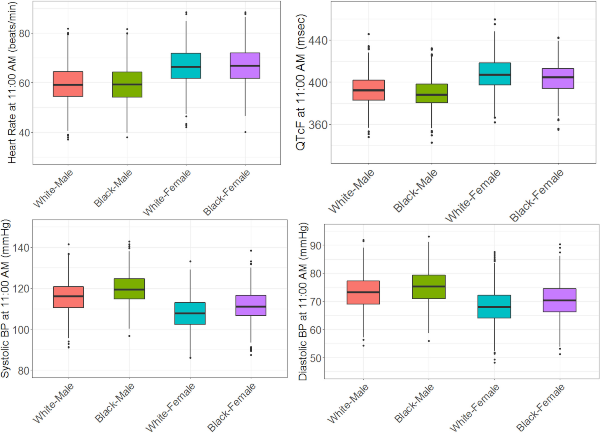
Does your study call for recurrent measurement of heart rate or blood pressure? If so, read “Models of Variability and Circadian Rhythm in Heart Rate, Blood Pressure, and QT Interval for Healthy Subjects Who Received Placebo in Phase I Trials” by Mukul Minocha et al. In this creative approach to characterize the sources of interindividual variability in key cardiovascular study measurements, the authors used nonlinear mixed-effects modeling with cosine functions to capture circadian oscillations in longitudinal clinical data from 1,035 healthy adult volunteers participating in phase I studies. Turns out gender, race, age, and body weight are significant contributors, but so is the time of day. This should come as no surprise since many of our biologic functions are governed by our so-called “internal clock,” otherwise known as a circadian rhythm. If you don’t believe in the importance of an internal clock, please consult 2017 Nobel Prize Laureates Jeffrey C. Hall, Michael Rosbash and Michael W. Young. If you want to take advantage of our understanding of the effects of circadian rhythm on cardiovascular study parameters and differentiate true drug-related treatment response or safety signal from inherent diurnal variability, read on.
Image by Minocha et al. Clin. Trans. Sci., https://ascpt.onlinelibrary.wiley.com/doi/10.1111/cts.12640, is licensed under CC BY-NC-ND 4.0. ©2019 AbbVie Inc.

The comment feature is locked by administrator.